How to Remineralize Teeth Naturally: My Son’s Enamel Hypoplasia Story
What enamel hypoplasia looks like, why it happens, and how teeth can heal
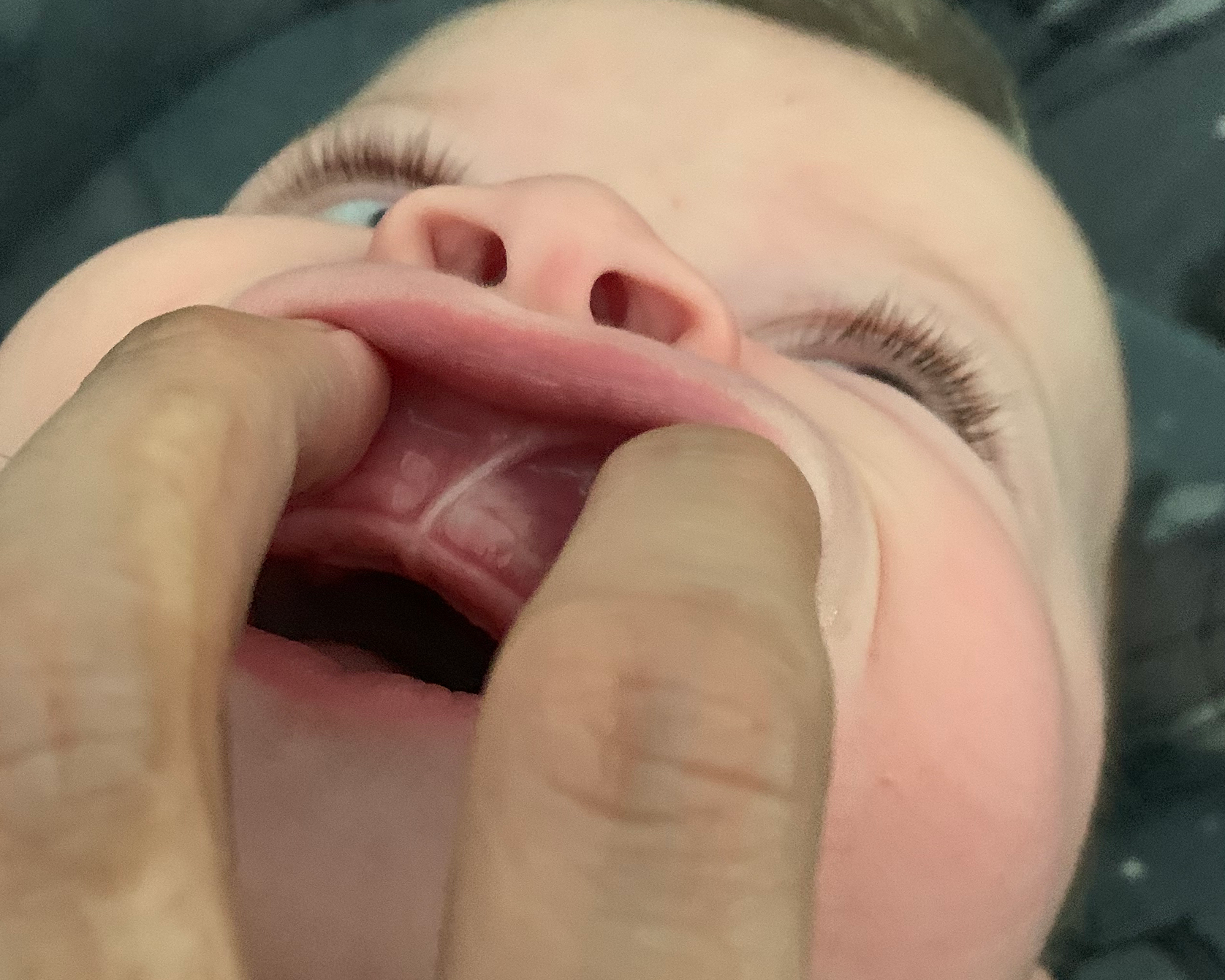
When my youngest was 8 months old, his first teeth began to come in. Like most parents, I expected them to be smooth and white, but instead they looked different. His front teeth were slightly transparent with areas of discoloration, almost splotchy in appearance. Right away, I knew something wasn’t right.
I started to wonder what could cause this so early. I brushed his teeth. I breastfed him. I cared for him in every way I knew how. How could new baby teeth already look damaged? At the same time, I noticed he had a large lip tie connecting between his front teeth. Some of the research I found online suggested that lip ties could trap milk and lead to decay, which left me questioning whether breastfeeding itself was harming his enamel.
What I later learned was that my son had a condition called enamel hypoplasia. This is when the enamel does not form properly, leaving teeth more vulnerable to sensitivity, cavities, and visible defects. Our journey with enamel hypoplasia is what led me to study tooth remineralization in children and eventually find a way to naturally support and strengthen his teeth. This is not medical advice, but it is our story, and my hope is that it gives other parents clarity and direction if they are facing the same questions.
What is Enamel Hypolasia?

Enamel hypoplasia is a developmental defect where the enamel — the protective outer layer of the tooth — does not form correctly. Instead of being smooth and strong, the enamel may be thin, patchy, or missing altogether.
In children, enamel hypoplasia often looks like:
-
White, yellow, or brown spots
-
Chalky or translucent patches
-
Rough textures, pits, or grooves
-
Teeth that chip or wear down easily
Enamel acts as a protective barrier for teeth. When that layer never fully develops, the softer dentin underneath can be exposed. This can cause chipping, sensitivity, and make teeth feel painful even with gentle brushing.
Early Signs of Enamel Hypoplasia in Baby Teeth
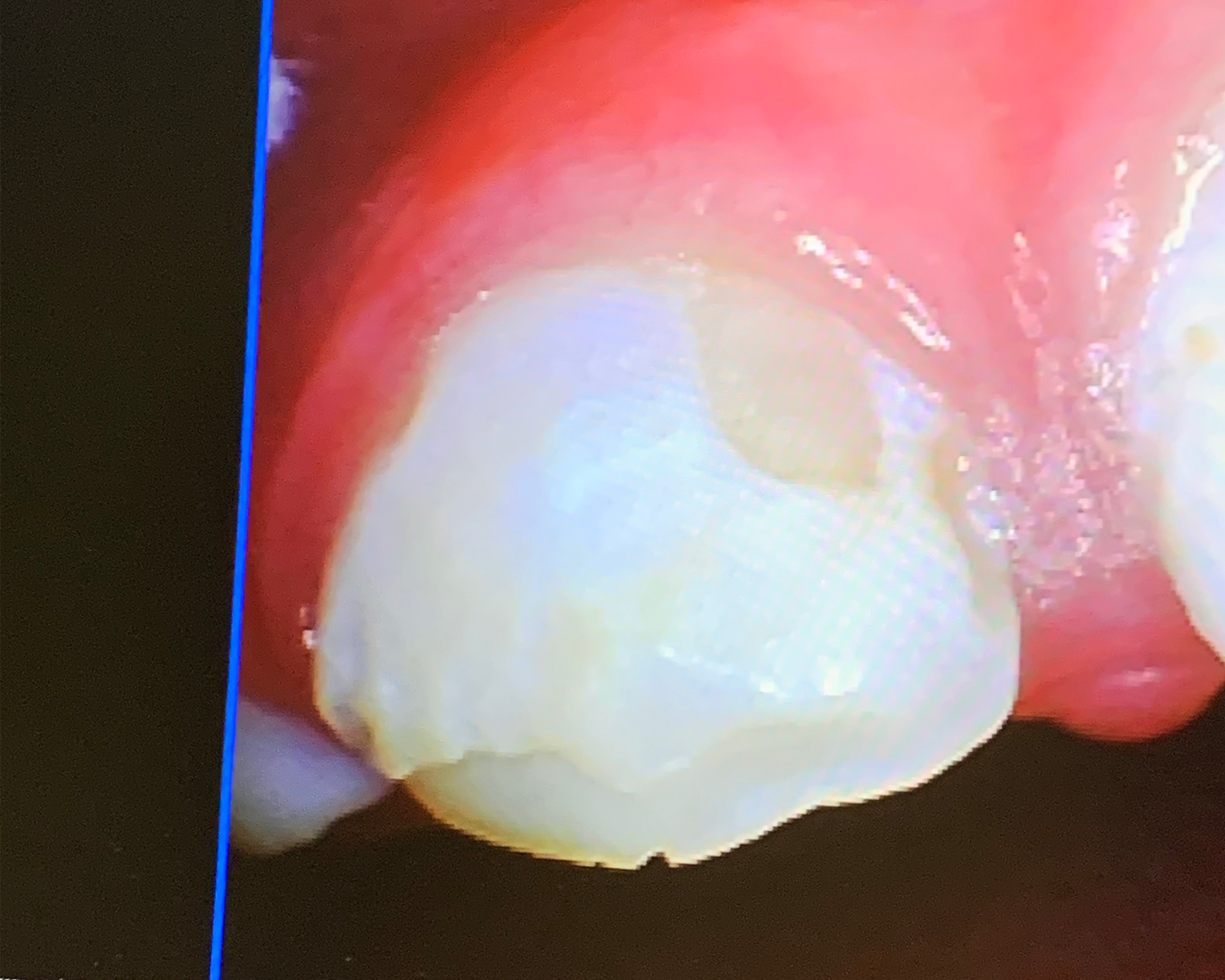
The first changes I noticed after his teeth erupted weren’t dramatic at a distance, but up close they looked unusual. Instead of smooth white enamel, the edges looked glassy and thin, with uneven patches of color. I wasn’t sure if it was my eyes playing tricks, so I used my camera to zoom in and check every angle. Looking back, those photos showed the earliest evidence of enamel hypoplasia — fragile enamel that had never fully formed.
As I tried to make sense of it, I kept asking myself why this had happened. Enamel begins forming in the second trimester of pregnancy and continues after birth while baby teeth are still developing under the gums. That means any stressor during those windows can leave a permanent mark on the enamel. Research shows contributing factors may include maternal illness or nutritional deficiencies during pregnancy, premature birth, low birth weight, early fevers in infancy, or certain medications such as repeated antibiotics.

My son spent his earliest days in the NICU. Preventative antibiotics were necessary at the time, and I will never know whether that, or something in pregnancy, set the stage for his enamel hypoplasia. What I do know is that from the very beginning, his enamel was compromised, and that close-up photo captured the earliest signs of just how vulnerable his teeth really were.
There is also research to support this connection. Several studies have shown that early antibiotic use and systemic illness in infancy can disrupt the way enamel mineralizes, leaving it thinner or weaker than it should be. For parents, the important takeaway is that enamel hypoplasia isn’t caused by brushing or diet, but by how enamel forms during critical windows of development.
-
Possible causes: Prenatal illness, low maternal mineral or nutrient status during pregnancy, premature birth, low birth weight, early fevers, or antibiotics.
-
What it looks like: White, yellow, or brown spots; chalky patches; pits or grooves; teeth that chip easily.
-
Why it matters: Weak enamel exposes dentin, causing sensitivity, cavities, and risk of infection.
-
What can help: A holistic dentist who understands remineralization, nutritional support (vitamins, minerals, probiotics), and trusting your gut when something feels wrong.
Lip Ties, Breastfeeding, and Enamel Health
Lip ties are often one of the first explanations given when a child’s teeth look weak or discolored. The common theory is that a restrictive lip tie traps milk against the upper front teeth, increasing the risk of decay. This idea is repeated widely, but it has never been proven as a primary cause of enamel defects. Many mothers are told their child’s teeth are damaged because they breastfed with a lip tie, which can feel like unfair mom-shaming rather than a clear medical answer.
The Lip Tie Theory Explained
- Pooling of milk: A tight lip tie may prevent the lip from lifting, which can trap milk and make cleaning harder.
- Hygiene challenges: Food or milk residue could linger longer, increasing risk for cavities.
What Research Actually Shows
- Enamel hypoplasia develops before a tooth erupts, during pregnancy and early infancy. It cannot be caused by milk sitting on a tooth that hasn’t fully formed yet.
- Lip ties may affect feeding and oral hygiene, but they are not considered a root cause of weak or missing enamel.
- Studies highlight prenatal health, nutrient status, prematurity, illness, or antibiotics as more consistent risk factors
Lip ties are real, and they can cause significant issues with feeding, oral function, and dental hygiene. A frenectomy can often make nursing easier, reduce discomfort, and support healthier oral development. But it is misleading — and unfair to mothers — to say that lip ties are the root cause of enamel hypoplasia. Enamel hypoplasia is a developmental defect that begins before teeth erupt. Suggesting that breastfeeding with a lip tie is the reason for weak enamel shifts blame onto moms instead of pointing to the medical and developmental factors that actually shape enamel.
For me, the lip tie was part of the journey because I wanted to explore every possible contributor. That’s why we decided to proceed with a frenectomy. At that appointment, I asked directly about the transparency and discoloration I had been seeing, but under the bright office lights the dentist told me everything looked fine. I left feeling unsettled, but hopeful the procedure might help. Looking back, I can see that the weak enamel I noticed was connected to early development, not to milk pooling under his lip.
Post Frenectomy: His Enamel Hypoplasia Became Worse

TTwo months post-frenectomy, the decline in his teeth was undeniable. The edges chipped away into jagged points, and the splotches that once looked faint grew darker and more widespread.
Everyday care turned into a struggle. Brushing his teeth caused him pain. He cried and fought us at every attempt, and we often had to hold him still just to clean his teeth. For him it was traumatic, and for us it was heartbreaking.
Where healthy enamel can absorb pressure and protect dentin, defective enamel breaks under the stress of chewing and brushing. Once dentin is exposed, the tooth becomes extremely sensitive, and even routine cleaning can feel painful.
These months were some of the hardest in early motherhood. I questioned myself constantly, wondering if there was something I had missed. What kept me going was the determination to keep searching for answers. I didn’t want to accept that his teeth would just keep breaking down.
Finally Getting Answers: An Enamel Hypoplasia Diagnosis
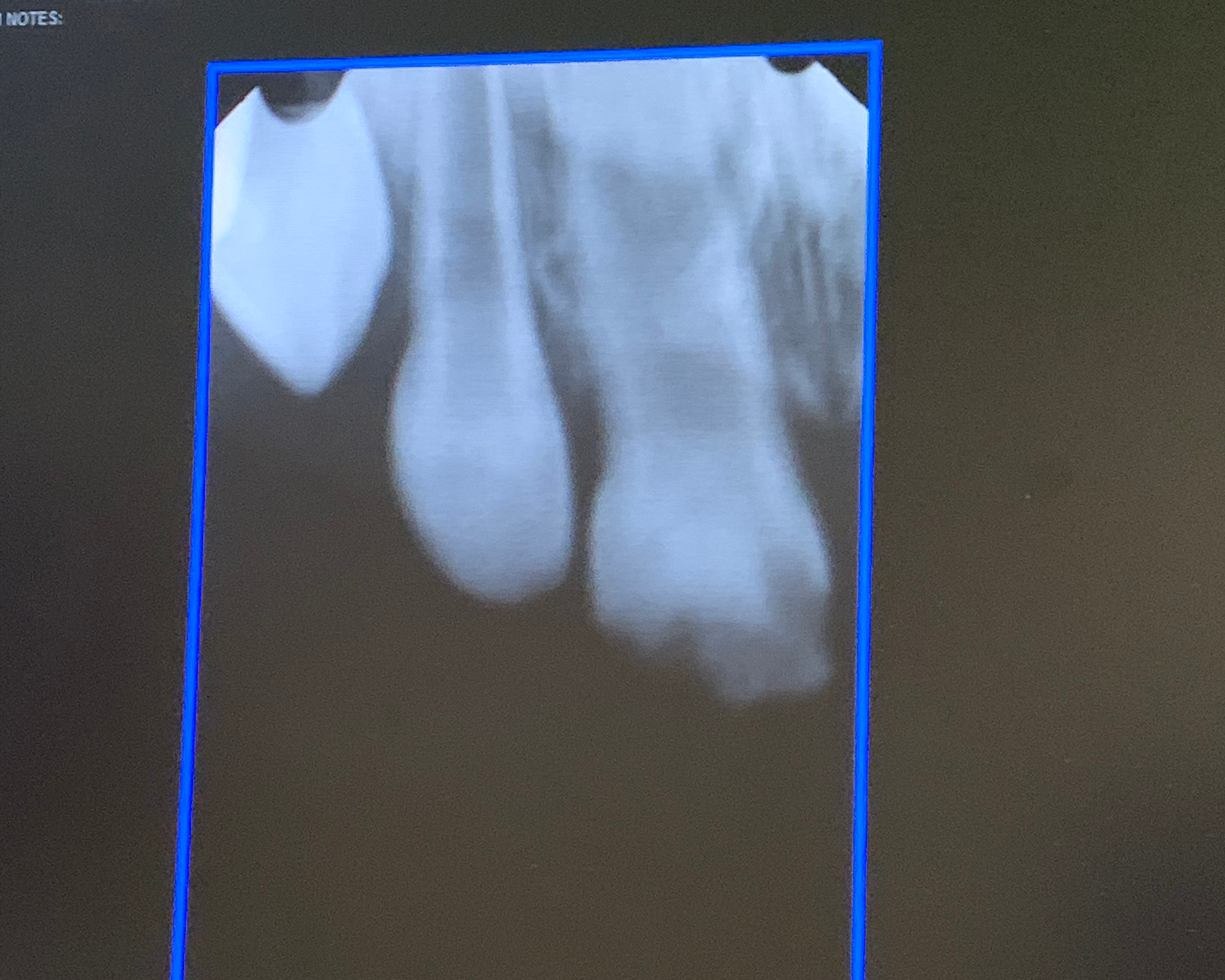
The turning point came when I brought him to a holistic dentist. For the first time, someone looked past the surface and used special intraoral cameras along with X-rays. What we saw was devastating — his enamel wasn’t simply worn down, it was missing in large areas. In places, the dentin was fully exposed, which explained why brushing caused so much pain.
This dentist explained what others had overlooked: the dentist confirmed what I had suspected all along: it was enamel hypoplasia, a condition where the enamel never forms correctly. She walked me through how this differs from decay, why it can’t be brushed away or blamed on hygiene, and how early-life factors like antibiotics or prenatal stress could have contributed. For the first time, the pieces began to make sense.
The dentist sat me down and laid out two very different paths forward.
Option 1: Caps. She explained that stainless steel or zirconia crowns could be placed over the damaged baby teeth. These caps are common in pediatric dentistry because they immediately cover weak enamel, restore function, and protect against further breakdown. The upside is quick protection; the downside is significant dental work at such a young age, with teeth he would eventually lose anyway.
Option 2: Remineralization. Instead of covering the problem, this path aimed to strengthen what enamel remained and encourage rebuilding through nutrition, supplementation, and topical therapies. It would take patience and consistency, and there were no guarantees, but it aligned more with a whole-body approach to healing.
Hearing these options was overwhelming. One choice promised quick results but felt invasive; the other was slower and uncertain, but seemed to address the root of the problem. In the end, we chose remineralization. My son was only 14 months old, and the idea of capping his baby teeth felt extreme. If there was even a chance to strengthen and protect them naturally, I wanted to try. I believed his enamel needed systemic support, not just a surface-level fix.
Starting Remineralization: Everything We Tried
I quickly discovered that advice online was overwhelming and conflicting. Some said remineralization was impossible. Others suggested strict, complicated protocols that didn’t seem realistic for a toddler. We had to find a balance between what was safe, what was doable, and what might actually work.
Here are some of the things we tried, but not everything worked for us. I am including this list as there is a lot of great information on each of these as to why it can help with remineralization, and although they didn’t work out for us, it doesn’t mean they aren’t worth looking into. Our biggest obstacle was my son’s age and willingness to take supplements that ultimately limited us.
- Iodine
- CariFree CTx3
- Fish Oil
- Bone Broth Protein Powder
- Probiotic for Teeth
- Silicea Cell Salts
- Calc Fluor
- Butter Oil
- Mineral Toothpaste
- MI Paste Plus
Not all of these stuck. With such a young child, there was no perfect protocol to follow, so we experimented with what we found online and tried just about everything to see what was possible. Some products weren’t realistic, some he flat‑out refused, and others became battles we had to let go. Through that process of trial and error, we eventually narrowed it down to what we could consistently manage and keep part of his daily routine.
Teeth Remineralization: The Protocol We Used
This is the protocol we committed to and followed every night:
Oral-health Probiotic
Oral-health specific probiotics are different from the typical gut probiotics you often hear about. Instead of colonizing the digestive system, they settle in the mouth and help shape a healthier oral microbiome.
This matters because the mouth is the first line of defense: balanced bacteria reduce harmful acid production, limit sticky biofilm, and create conditions that support enamel remineralization.
Certain strains, like Streptococcus salivarius M18, even produce natural enzymes that loosen plaque buildup around the teeth. Research also suggests oral probiotics may support immune and respiratory health, which adds another layer of benefit for kids.
For children with enamel hypoplasia, oral-health probiotics can be especially helpful because they lower the everyday bacterial pressure on already vulnerable teeth. By giving the mouth friendlier bacteria to work with, you reduce the burden on weak enamel and make it easier for minerals to rebuild where they’re needed.
What we used: Hyperbiotics Vital Nutrients Pro Kids Probiotic ENT
Our Routine: 1 tablet nightly
Vitamin D3
Vitamin D is essential for calcium absorption and mineralization. Without enough vitamin D, the body cannot properly use the calcium and phosphorus that teeth need to harden. Research has shown that deficiency in early childhood is linked not only to enamel defects but also to a higher risk of cavities and weaker bone development overall.
We split his intake between two supplements, giving 1,000 IU from this gummy of plain D3 (1,000 IU) and another gummy of his D3 + B12 supplement (1,000 IU of D3) for a total of 2,000 IU per day.
Raising his dose made sense because vitamin D acts almost like a switch: without it, minerals cannot integrate into enamel, but with it, the body can build and repair stronger tooth structure.
It also supported his immune system and overall bone health, which were key factors while his teeth and jaw were still developing.
What we used: Mary Ruth Organics Vitamin D3 Gummies
Our Routine: 2 gummies nightly for 2000 IU of D3
*Now that my son’s are older and able to swallow capsules, we have switched to Designs for Health D3 + K2
Designs for Health is also the Vitamin D3 + K2 that my husband and I personally use as I am a huge advocate of D3 in our supplement rotation.
Fish Oil
Omega‑3 fatty acids (EPA and DHA) help regulate inflammation in the mouth and support gum and other soft tissues. By lowering chronic inflammation, they can reduce gingival swelling and bleeding and keep the dental biofilm less aggressive.
For remineralization specifically: omega‑3s do not directly “build” enamel, but they help create the conditions enamel needs to reharden — calmer gums, a more neutral saliva environment, and less acid pressure from the biofilm. Early clinical and laboratory research shows omega‑3s can down‑regulate inflammatory mediators in oral tissues and may limit the activity of acid‑producing bacteria. That means less ongoing demineralization and a better chance for minerals to move back into the tooth surface.
Omega‑3s also provide a fat source that can improve absorption of fat‑soluble vitamins (A, D, K). Taking vitamin D with dietary fat can enhance uptake, which matters because vitamin D regulates how the body uses calcium and phosphate for enamel and bone.
What we used: Nordic Naturals Children’s DHA
Our Routine: 1 serving nightly
Mineral Toothpaste
We used a mineral-rich toothpaste that combined natural ingredients instead of fluoride.
Its base of calcium carbonate and bentonite clay provided gentle polishing and a direct source of minerals to the tooth surface.
Colloidal silver and sea salt acted as natural antimicrobials, while xylitol helped reduce cavity-causing bacteria by lowering acidity in the mouth.
Castile soap provided mild cleansing, and trace minerals, spirulina, and moringa leaf offered additional micronutrients to support oral health.
Essential oils like juniper berry, rosemary, peppermint, and pine gave antibacterial properties and a fresh taste, while iodine added another layer of microbial support.
Together, these ingredients created an environment that supported remineralization by neutralizing acids, reducing harmful bacteria, and supplying minerals directly where his enamel was fragile.
What we used: Nelson Naturals Moringa Mineral Toothpaste
This is currently showing unavailable on Amazon as of the time of writing this, I will keep an eye out for it.
Our Routine: Brushed twice daily
Silicea
Silica is a trace mineral that plays a role in the formation and maintenance of connective tissue, bone, and enamel integrity. It helps the body use calcium and other minerals effectively, acting almost like a scaffolding that minerals attach to when rebuilding and strengthening enamel.
In protocols for supporting teeth, silica is often used to encourage stronger enamel and reduce brittleness by reinforcing the underlying structure.
For us, adding it was a way to strengthen the framework his enamel needed to stay resilient, and over time it became a consistent part of his routine.
What we used: Hylands Cell Salt #12 Silicea 6X
Our Routine: x2 Tablets sublingually nightly
Calc Fluor
Calc Fluor is a homeopathic mineral salt made from calcium fluoride. It is not the same as conventional fluoride treatments used in dentistry. Conventional fluoride is usually sodium fluoride or stannous fluoride, applied topically in toothpaste or treatments to harden the outer enamel surface.
Calc Fluor, by contrast, is taken orally in micro‑doses as a cell salt. Instead of coating the teeth, it is intended to support the structural framework of enamel and connective tissues from within the body.
The key difference is that Calc Fluor works systemically. It provides calcium and fluoride ions in a form that aligns with mineral pathways inside the body, supporting long‑term resilience of enamel, bones, and ligaments.
This is different from topical fluoride, which works locally on the surface of teeth. For children with enamel hypoplasia, Calc Fluor has been used in holistic protocols to help reduce brittleness and encourage stronger, less fracture‑prone enamel.
For us, adding Calc Fluor was another way to reinforce weak enamel from within. Over time, we noticed his teeth looking and feeling more solid, which gave us confidence to keep it in his routine.
What we used: Hylands Cell Salt #1 Calc Fluor 6X
Our Routine: x2 Tablets sublingually nightly
Watching His Teeth Heal After Remineralization

Within 3 months, I saw something I’ll never forget: the areas of exposed dentin began to look like they were filling in. The new enamel came in yellow at first, which worried me. Then I came across another mom’s story describing the exact same process in her daughter — that gave me the reassurance I needed to stay the course.
By 5–6 months, his teeth had filled in completely. They weren’t white, but they were solid and strong. Over time the yellow areas darkened into brown as the old, weak enamel on top died away while healthier enamel was establishing underneath. It was almost like watching the tooth shed its fragile shell so something sturdier could take its place.
That other mom’s experience helped me frame what I was seeing. She described how her daughter’s teeth first improved, then turned darker and darker brown. A holistic dentist later explained to her that the brown “crust” was actually dead, fragile enamel on the outside, while new enamel had grown underneath. Once the old layer was buffed away, the dentist confirmed the teeth had completely remineralized. Knowing her story gave me hope that the yellow and brown phases weren’t failure, but part of the healing process.
For parents, this stage can be confusing and even distressing. Enamel that is healing does not always look prettier at first. Yellow or brown changes often mean that weak enamel is dying off while stronger enamel is forming below. In some cases, dentists can smooth or polish away the dead layer once the new enamel has hardened underneath. The key takeaway is that color changes do not always mean decay.
After one year, the enamel was hard and stable, even if the color stayed yellow or brown. Because he was so young when we started, you could actually see a line — the portion of his tooth that had grown during remineralization looked healthier than the part that formed before.

AT THE START

3 MONTHS LATER

6 MONTHS LATER

11 MONTHS LATER

13 MONTHS LATER
Restoring Function and Appearance of His Teeth
When my son was 4.5 years old, we returned to the dentist for an important check‑in. By then, his enamel had become strong and stable, but the surface was uneven from the years of breakdown and regrowth. The dentist decided the best approach was to rebuild and protect his teeth with a restorative procedure.
She first smoothed away rough, jagged edges and then applied a tooth‑colored resin bonding material. This process is very similar to a filling, but instead of repairing a cavity, it was used to reinforce the fragile enamel and restore the tooth’s original shape. The resin was layered directly onto the teeth, cured with a special blue light to harden it, and polished so that the surface looked smooth and natural.
In some ways, it functioned almost like a thin veneer, covering weak enamel and making the teeth appear whole again.
I want to be clear: This procedure would NOT have been possible if the teeth weren’t completely hard and healed. If there was any softness or decay, they would not have done this procedure. Despite the appearance of color, his teeth had healed.


Why This Procedure Mattered
-
Protection: Bonding sealed areas where enamel was thin, shielding dentin.
-
Appearance: For the first time in years, his front teeth looked brand new. He left the appointment smiling, with teeth that finally looked like they belonged to him.
For a child who had spent years hiding his teeth, the change was life‑changing. And for us as parents, it was the visible proof that all of the daily effort we had poured into remineralization had created a foundation strong enough for restoration.
Looking Back and Looking Ahead
This journey taught me that enamel hypoplasia is not the result of parental failure. It is a developmental condition shaped long before brushing or diet play a role. Remineralization is not always easy, and it is not guaranteed, but in our case it gave my son back his smile and his confidence.
Now we are focused on the next chapter: supporting his airway, addressing his crossbite, and guiding his jaw development. But the lessons I learned through his remineralization journey — persistence, advocacy, and education — will always stay with me.

BEFORE WE STARTED TREATMENT IN THE PROGRAM TO
CORRECT HIS JAW AND AIRWAY

9 MONTHS INTO TREATMENT FOR THE PROGRAM TO
CORRECT HIS JAW AND AIRWAY
his is our personal story and what worked for us. It is not medical advice. Always consult with your dentist or healthcare provider for individualized care.
🛒 Some of the products we share may include Amazon affiliate links. If you purchase through those links, I may earn a small commission at no additional cost to you. Thank you for supporting our work and helping us keep sharing resources with families.